Treatment of Maple Syrup Urine Disease (MSUD)
Treatment of children with MSUD must be started as soon as possible. This involves a complex approach to maintain metabolic control. A special, carefully controlled diet is the focus of daily treatment. Prompt treatment is needed to prevent brain damage and other serious medical problems.
The 2 main aspects of the treatment of MSUD are long-term management (diet) and the treatment of episodes of acute metabolic decompensation (diet and possible IV therapy). Fortunately, with adherence to the dietary restrictions and regular medical checkups individuals with MSUD can live long and relatively healthy lives.
Diet

Long term treatment requires a special, low-protein diet. When the condition is diagnosed, and during acute episodes, treatment involves eating a protein-free diet; fluids, sugars, and possibly fats are given through a vein (IV).
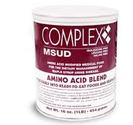
The diet for babies includes a man-made formula with low levels of the amino acids leucine, isoleucine, and valine (also known as the branched-chain amino acids). Your metabolic doctor and dietician will tell you what type of formula is best and how much to use.
In addition to a low-protein diet, children are often given a special medical formula as a substitute for milk. This formula gives them the nutrients and protein they need while helping keep their branched-chain amino acid (BCAA) levels in a safe range. The diet is also made up of foods that are very low in the BCAAs. This means your child will need to avoid foods such as cow’s milk, regular formula, meat, fish, cheese and eggs. Regular flour, dried beans, nuts, and peanut butter also have BCAAs and must be avoided or strictly limited. Many vegetables and fruits have only small amounts of the BCAAs and can be eaten in carefully measured amounts. There are other medical foods such as special low-protein flours, pastas, and rice that are made especially for people with MSUD. Some states offer help with payment, or require private insurance coverage for medical formula and other special medical foods. Your metabolic doctor and dietician will decide on the best food plan for your child. The exact plan will depend on many things such as your child’s age, weight, and general health. Your dietician will fine-tune the diet over time. Any diet changes should be made under the guidance of a dietician..
The diet for babies includes a man-made formula with low levels of the amino acids leucine, isoleucine, and valine (also known as the branched-chain amino acids). Your metabolic doctor and dietician will tell you what type of formula is best and how much to use.
In addition to a low-protein diet, children are often given a special medical formula as a substitute for milk. This formula gives them the nutrients and protein they need while helping keep their branched-chain amino acid (BCAA) levels in a safe range. The diet is also made up of foods that are very low in the BCAAs. This means your child will need to avoid foods such as cow’s milk, regular formula, meat, fish, cheese and eggs. Regular flour, dried beans, nuts, and peanut butter also have BCAAs and must be avoided or strictly limited. Many vegetables and fruits have only small amounts of the BCAAs and can be eaten in carefully measured amounts. There are other medical foods such as special low-protein flours, pastas, and rice that are made especially for people with MSUD. Some states offer help with payment, or require private insurance coverage for medical formula and other special medical foods. Your metabolic doctor and dietician will decide on the best food plan for your child. The exact plan will depend on many things such as your child’s age, weight, and general health. Your dietician will fine-tune the diet over time. Any diet changes should be made under the guidance of a dietician..
As the person grows to adulthood, he or she must always watch their diet, avoiding high protein foods such as meat, eggs, and nuts. Persons with this condition must remain on this diet permanently.
It is very important to always follow this diet to prevent nervous system (neurological) damage. This requires frequent blood tests and close supervision by a registered dietitian and physician, as well as cooperation by parents.
It is very important to always follow this diet to prevent nervous system (neurological) damage. This requires frequent blood tests and close supervision by a registered dietitian and physician, as well as cooperation by parents.
Supplements
Vitamins are organic substances required by the body in small amounts for various metabolic processes. Vitamins may be synthesized in small or insufficient amounts in the body or not synthesized at all, thus requiring supplementation.
Children with a rare form of MSUD, called “thiamine-responsive MSUD”, can often be helped by thiamine supplements. Some children with classic MSUD may also benefit from thiamine. Ask your doctor whether or not your child should take thiamine supplements. Do not use any supplements without checking with your doctor.
Children with a rare form of MSUD, called “thiamine-responsive MSUD”, can often be helped by thiamine supplements. Some children with classic MSUD may also benefit from thiamine. Ask your doctor whether or not your child should take thiamine supplements. Do not use any supplements without checking with your doctor.
Dialysis
The health care provider will follow the BCAA levels closely, and will adjust the diet based on amino acid levels. In rare circumstances, hemodialysis or peritoneal dialysis is required to remove BCAAs and keto acids.
Gene Therapy
Gene therapy is also a potential future treatment for patients with MSUD. This would involve replacing the mutated gene with a good copy, allowing the patient's cells to generate a functional BCKD protein complex and break down the excess amino acids.
Liver Transplant
A liver transplant is an optional treatment. The BCKAD enzyme that causes MSUD is located in the liver. A donor liver from a person who does not have MSUD has enough enzyme activity to allow the person with MSUD to live free of the affects of the disease. After transplant, the person with MSUD still carries the gene for the disorder, which can be passed to their offspring, but they are no longer in danger of a metabolic crisis and can eat a normal diet.
Successful liver transplants in patients with classic MSUD have been reported. However, this is a major surgical procedure with risks and potential long-term complications of liver transplantation in contrast to the beneficial low-risk dietary therapy that has equally good outcome. Many factors must be considered before surgery and this option should be discussed very thoroughly with your child's physicians.
Successful liver transplants in patients with classic MSUD have been reported. However, this is a major surgical procedure with risks and potential long-term complications of liver transplantation in contrast to the beneficial low-risk dietary therapy that has equally good outcome. Many factors must be considered before surgery and this option should be discussed very thoroughly with your child's physicians.
When to Call Your Doctor

For children with MSUD, even minor illness can cause a metabolic crisis. In order to prevent problems, call your doctor right away when your child has any of the following:
- decreased liquid intake
- poor appetite
- low energy or extreme sleepiness
- vomiting
- diarrhea
- any infection or illness
- a fever
- behavior or personality changes
- difficulty walking or balance problems
Children with MSUD need to eat more carbohydrates and drink more fluids during any illness – even if they’re not hungry – or they could have a metabolic crisis. Children who are sick may not want to eat. If they can’t eat, or if they show signs of a metabolic crisis, they may need to be treated in the hospital.
Ask your metabolic doctor if you should carry a special travel letter with medical instructions for your child’s care.
- decreased liquid intake
- poor appetite
- low energy or extreme sleepiness
- vomiting
- diarrhea
- any infection or illness
- a fever
- behavior or personality changes
- difficulty walking or balance problems
Children with MSUD need to eat more carbohydrates and drink more fluids during any illness – even if they’re not hungry – or they could have a metabolic crisis. Children who are sick may not want to eat. If they can’t eat, or if they show signs of a metabolic crisis, they may need to be treated in the hospital.
Ask your metabolic doctor if you should carry a special travel letter with medical instructions for your child’s care.
